IDS071 - Neurocritical care in Intensive Care Units in Canada
Catégories
Les projets ou stages publiés auxquels vous accédez sont des rapports d'étudiants et doivent être pris comme tels. Il peuvent donc comporter des imperfections ou des imprécisions que tout lecteur doit admettre et donc supporter. Il ont été réalisés pendant les périodes de formation et constituent avant-tout des travaux de compilation bibliographique, d'initiation et d'analyse sur des thématiques associées aux concepts, méthodes, outils et expériences sur les démarches qualité dans les organisations ou sur les technologies en santé.
Si, malgré nos précautions, vous avez des raisons de contester ce droit de diffusion libre, merci de nous en faire part (master@utc.fr), nous nous efforcerons d'y apporter une réponse rapide. L'objectif de la présentation des travaux sur le web est de permettre l'accès à l'information et d'augmenter ainsi la qualité des échanges professionnels.
Nous ne faisons aucun usage commercial des travaux de projet ou de stage publiés, par conséquent les citations des informations et l'emploi des outils mis à disposition sont totalement libres. Dans ce cas, nous vous demandons de respecter les règles d'éthique en citant explicitement et complètement vos sources bibliographiques.
Bonne lecture...
Author
Contact
Citation
A rappeler pour tout usage - To quote for any use : ZAGHDOUDI Lina, « Neurocritical care in Intensive Care Units in Canada », Université de Technologie de Compiègne (France), Master Ingénierie de la Santé, Parcours Technologies Biomédicales et Territoires de Santé (TBTS) et Dispositifs Médicaux et Affaires Réglementaires (DMAR), Mémoire de stage, juillet 2020, https://travaux.master.utc.fr/formations-master/ingenierie-de-la-sante/ids071/
Résumé
Les facteurs humains ou l'ergonomie est l'étude de la façon dont les humains se comportent physiquement et psychologiquement par rapport aux environnements, aux produits ou aux services.
La conception d'interfaces est une discipline en évolution. L'interface de conception écologique (EID) combine des concepts d'humains et d'environnement, et le concept d'affichage.
L'analyse cognitive du travail (CWA) est un cadre formatif basé sur des contraintes pour analyser des systèmes sociotechniques complexes tels que les unités de soins intensifs. Le cadre CWA aide à développer des outils de support tels que, par exemple, une hiérarchie de l'abstraction (AH).
Dans ce rapport de stage, nous verrons ici comment la CWA est appliquée aux soins neurocritiques dans l'unité de soins intensifs à travers la conception d'une interface suivant l’EID.
Abstract
Human Factors or Ergonomics is the study of how humans behave physically and psychologically in relation to environments, products, or services.
Interface Design is an evolving discipline. Ecological Design Interface (EID) combines concepts of Humans and environment, and the concept of Display.
Cognitive Work Analysis (CWA) is a formative, constraint-based framework for analyzing complex sociotechnical systems such as Intensive Care Units. The CWA framework helps to develop support tools such as an Abstraction Hierarchy (AH).
This internship report focuses on how CWA can be applied to neurocritical care in the intensive care unit using EID.
Téléchargements - Downloading
Neurocritical care in Intensive Care Units in Canada
Internship Report :
Neurocritical care in Intensive Care Units
Acknowledgment
Over all, I would like to thank, professor Sofiane Boudaoud, professor Isabelle Claude and the educational team of Healthcare’s Engineering, including Professor Dan Istrate at the University of Compiegne, for giving me the great opportunity to do my internship in the scientific research area at a prestigious university such as the University of Waterloo. In addition, I am grateful to each and everyone for giving me basic engineering knowledge in the Healthcare field.
I would especially like to thank Professor Catherine Burns, my internship tutor, for her welcome at the AIDL team, for assisting me from the moment preceding the start of the internship and for supporting and encouraging me over time for the work I have done.
I would like to thank personally Ece Uereten, a PhD student who works with me on neurocritical care. Working with her was a great pleasure for me and her support made me progress without having any difficulties.
My special thanks are for the Secretariat of my master’s degree, the International Relations Department of the UTC, the IVGS department, the HR department of UW and Fran Hannigan, Vicky Lawrence, Audray Sloboda, Charlotte Amstrong, for helping me with all the administrative procedures during my internship.
I also owe a great debt of gratitude to Kirsten Anderson, Ryan Tennant, Olamide Olatoye, Murat Dikmen, Ramtin Lotfabadi and Fan He, members of my team, have always been kind, helpful and patient to help me and assist me to carry out the important tasks throughout the internship period.
Special thanks for my comrades, Philippe Portailler, Kawtar Ghiatt, Mariam Laghi Mrabat and Clara Magnier for giving me their feedbacks of their experiences at UW, for not only advising me but also helping me with all of the obstacles that I had to face coming to Canada.
I also thank my family and my friends for supporting and encouraging me along my journey away from them. Without their support I would not have been as motivated as I am now.
Abbreviations
- AH : Abstraction Hierarchy
- AIDL : Advanced Interface Design Lab
- CBB : Centre for Bioengineering and Biotechnology
- CPP : Cerebral Perfusion Pressure
- CSF : Cerebrospinal fluid
- CWA : Cognitive Work Analysis
- ConTask : Control Task (Analysis)
- EEG : Electro Encephalo Gram
- EID : Ecological Interface Design
- GCS : Glasgow Coma Scale
- HF : Human Factors
- HFES : Human Factors and Ergonomics Society
- ICU : Intensive Care Unit
- ICP : Intra Cranial Pressure
- IH : Intracranial hypertension
- MAP : Mean Arterial Pressure
- SARS : Severe Acute Respiratory Syndrome
- SHAP : SHapley Additive exPlanations
- SYDE : SYstem Design Engineering
- UW : University of Waterloo
- UXD : User Experience Design
- WDA : Work Domain Analysis
- WFH : Work From Home
Introduction
The world has known the biggest pandemic in 2020 due to Covid-19. According to the World Health Organization, a pandemic is defined as “an epidemic occurring worldwide, or over a very wide area, crossing international boundaries and usually affecting a large number of people”[1] [2]. By epidemic, we mean “a widespread occurrence of an infectious disease in a community at a particular time”[3].
Covid-19 is a new disease which has similar symptoms to common cold such as fever, dry cough, and tiredness. It spreads through close contact with an infected person. This coronavirus disease is caused by a virus called SARS-CoV-2. Coronaviruses are part of a large family of viruses that can cause illness in animals or humans. The spread of this new infectious disease began in Wuhan, China, in December 2019 and has reached today 216 countries, causing 495 760 confirmed deaths and more than 9 843 073 confirmed cases on June 27th 2020 [4]–[6].
Anyone can catch this disease without or with mild symptoms in most cases. However, Covid-19 can also evolve into severe respiratory illnesses, like pneumonia, with an occurrence of 1 infected person out of 5 [4]. Two categories of people are most likely to be affected by these severe symptoms, the elderly, and those with underlying conditions such as high blood pressure, heart and lung problems, diabetes or cancer. These persons need a hospital treatment and patient care in the ICU [7].
This has
shown the importance of having functional and efficient ICU units in order to
improve the quality of care given by physicians and nurses. Thus, it would be
interesting to think about how the Ecological Design Interface (EID) and
Cognitive Work Analysis (CWA) methods, could improve the quality of care.
I. Internship environment
1. The University of Waterloo
University of Waterloo, with its leading “spirit of the why not”, is a public research university created in 1957 by business leaders to address industry needs. Its particularity is that the inventor ownership of intellectual property, so it is an incentive way to attract leading and entrepreneurial researchers. It’s the largest post-secondary program in the world with the co-op Education.
- UW has reached the first rank of Comprehensive Research for 12 years consecutive years according the research info source 2019 [8], [9].
- It is also the most innovative university in Canada for 28 years [9], [10].
- And the first in the world for student-employer connections [9], [11].
University of Waterloo is composed by different schools such as Public Health and Health Systems, Accounting and Finance, Architecture, Planning, Computer Science, Optometry and Vision Science, Pharmacy, but also by different faculties : Applied Health Sciences, Arts, Engineering, Environment, Mathematics and Science.
2. The Faculty of Engineering
It’s Canada’s Largest Engineering School with more than 8000 undergraduate students, 13% international students and about 2000 graduate students.
The Faculty of Engineering is composed by 8 following departments :
- Electrical and computer engineering
- Mechanical and mechatronics engineering
- Systems Design Engineering
- Management Sciences
- Chemical engineering
- Civil and Environmental engineering
- School of architecture including integrated design
- Conrad School of Entrepreneurship and Business
They offer, among the mentioned departments, 15 bachelor degree programs and 37 graduate degree programs.

Here you can find the Waterloo Engineering Integration Complex in the campus in Figure 2. That aims to be intelligent, connected, digital and physical. The E7 Integration Hub is in Figure 1.

3. The System Design Engineering department
The department of SYDE was established 40 years ago and until today it is still providing the most flexible programs and various areas of research such as environmental socioeconomic and political aspects. Started in 1969, the department was considered unique due to the interdisciplinary programs with leading and developing topics. The distinctive nature of the offered programs within the department emerged from the topics covered in the curriculum. Topics covered include political, environmental, economic, social and technical aspects of engineering.
4. The Centre for Bioengineering and Biotechnology
In 2011, the UW established the centre CBB. Catherine Burns, my internship supervisor, was the founding Executive Director (ED) until May 2020. Since its establishment, CBB focused on facilitating tactical multidisciplinary research that connects technology to biosciences, health sciences and environmental sciences. Moreover, CBB strived to cover industrial challenges by holding events with companies, discussions and academic seminars and workshops. Financially, CBB uses independent funding system to supports researchers by applying to grants and seeking alternative funding opportunities.
Location
The Centre is located at 200 University Ave West, Waterloo, ON N2L 3G1 | East Campus 4 Building, Room 2001, in Figure 3.

The Staff and Leadership Organization
Since May 2020, Karim S. Karim became the new Executive Director of the CBB [12].
The CBB team is also composed by :
- Carly Turnbull, the project co-ordinator, interim manager, program Development and Partnerships
- Charlotte Armstrong, the administrative assistant
- Colin Russell, Manager, Program Development and Partnerships
- Catherine Burns, the founder and former CBB Executive Director
The product is knowledge transfer and partnerships.
Budget
The Centre’s budget is not part of the public domain, but financial statements about the University of Waterloo can be found here.
5. The Advanced Interface Design Lab
At UW, each faculty and department relate to laboratories. The AIDL is attached to SYDE. Catherine Burns, my supervisor, is the director of this lab.
The AIDL, focus on collaborative processes between technology and human users with the goal of developing advanced interfaces in the following domains :
- Defence and Aviation
- Financial Trading
- Healthcare
- Automated Vehicles
- Human Interaction with Artificial Intelligence
- Other Projects in Interface Design, Collaboration, and Visualization
6. My role in this internship : research assistant
During my internship, I was assigned the position of a research assistant. I worked on an ICU neurocritical care project with a Ph.D. student, Ece Uereten. Aside from my main project, I participated in a secondary project covering Artificial Intelligence in Finance. I covered the visualisation of SHAP[1] for a peer to peer lending website managed by Murat Dikmen.
In both projects, work was done in groups which sharpened my teamwork skills. Team meetings were done every week to provide updates about the progress of the project and to show the professional development acquired by team members. During each meeting, members would present challenges they faced and the skills they learned while working on the assigned projects. Moreover, the meetings were used to discuss future steps and tasks for each member.
My role as
a research assistant was affected by Covid-19 thus restricting my
responsibilities to mainly conducting literature reviews, requesting supplies
necessary for the project, attending online project meetings, attending an international
conference HFES symposium, and summarizing project results through presentations.
II. Neurocritical care in ICU
Neurocritical care is a medical area that deals with the treatment of serious diseases in the nervous system and identifies, prevents and treats them. Neuro-ICU is the place where the patients are admitted and taken care of.
1. Intensive Care Units in Canada
The intensive critical care unit provides intensive care to severely ill patients. According to a report, in 2013–2014, 11% of the more than 2 million adult hospital stays in Canada are spent in an ICU (outside Quebec) [13].
The average daily cost of an ICU stay is estimated to be as high as 3 times the average cost of a day’s stay in a general ward. This is because ICU stays are more resource-intensive in terms of personnel to equipment and medication. For these reasons, it is important to better understand the use of this constrained resource with respect to operating patterns, patient flow, trends in admissions, patient populations and process of care for those treated in ICUs [13].
There are three different types of ICUs :
- The general ICUs
- The specialized ICUs : for example, neuro-ICU
- The paediatric ICUs
Nonetheless, it could also be a combination of the any of the above types.
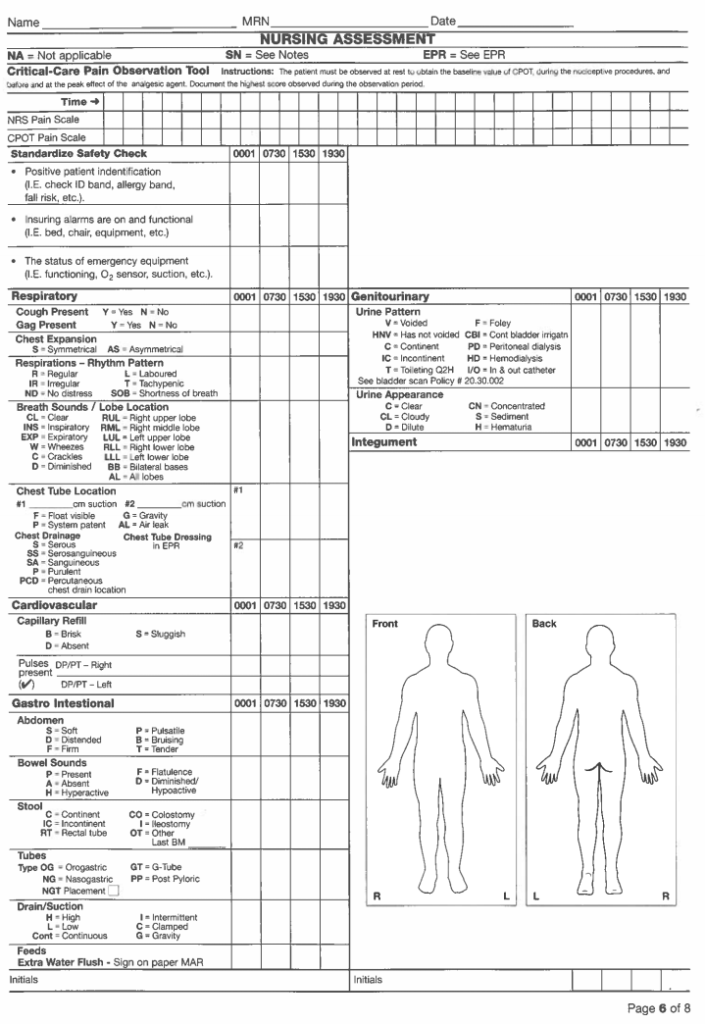
In ICUs, a lot of medical devices are connected to the patients. There is a lot of data obtained from patients through monitors, ventilators, EEG etc. Nurses perform their care oversight using a flowsheet aspresented in Figure 5. They note down data related to cardiovascular, respiratory, neurologic, nursing care, nursing assessment, clinical notes and fluid balance. Although this flowsheet is thorough it presents limitation such as the multitude of variable parameters that need to be taken into account. Another limitation is the lack of continuous tracking of a patient's vitals. As a result, physicians do not get the complete picture of the patient's history. The patient's life can be at stake for a few minutes or even seconds for patients in neurocritical care. The main issue is to track data continuously and show data on one screen. It will aid physicians in storing those data.
As it is shown in Figure 6, the ICU is a complex dynamic socio-technical environment. Numerous interactions between patients and caregivers take place, as well as interactions of the patients with support staff such as pharmacists and technicians. Caregivers are changing. Similarly, the patient’s conditions change as well. For example, a nurse takes care of the patient and take notes in the flowsheet. Then, the physician threatens the disease of the patient in critical conditions. Afterwards, the patient is connected to several medical devices. All these interactions should be taken into account in our EID.
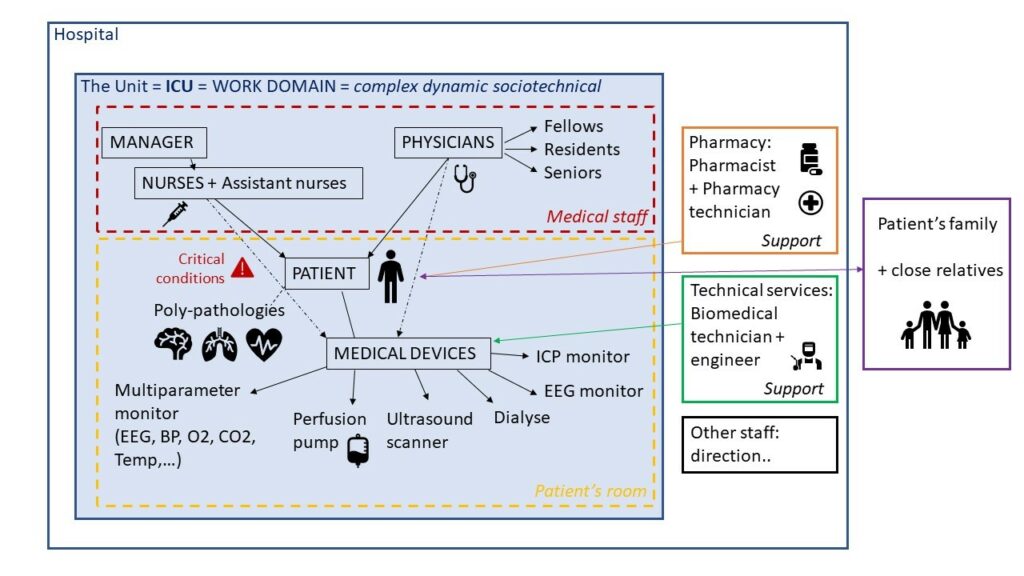
Thus, we are investigating whether integrating the information from a range of medical devices into an integrated display in Neuro-ICU using EID would be efficient. This integrated display could be dynamic or static. This EID should facilitate decision-making for healthcare personnel.
2. EID and CWA modelling
Ecological Design Interface
The word ecological deals with the relationship between humans and the environment. Interface design relates to the display. EID is known for visualizing functional relationships in a “quick glance” with little cognitive efforts. The motivation for EID originated from problems arising in the interface design of complex socio-technical systems. It could be applied to neurocritical care in ICU.
Why choose EID instead of UXD ? UXD is a user-centered windows-based interface whereas EID takes a wider account of the environment. It bridges between humans and the program/environment. An understanding of human conception, cognition, and behaviour is critical to designing interfaces. That much can be learned by getting feedback from actual users of the interface, at the early design stages, and then through testing various points in the design [14].
EID approach is used : when asking users is not possible, when we want users to become experts and when we want to handle the unexpected [14].
In complex systems, it is useful to understand how the system works, before beginning the design [14]. There are two key concepts in EID from cognitive engineering research : the Abstraction Hierarchy (AH) and the Skills, Rules, Knowledge (SRK) framework. That is why the CWA approach was our first step.
Cognitive Work Analysis
As previously mentioned, ICU is a complex dynamic socio-technical system therefore, to understand how ICU works and its constraints, we used CWA modelling. It allowed us to understand physicians but also to focus on the workload.
The word cognitive is associated with human factors or ergonomics. The word work is related to a world, not a task. Analysis refers to a modelling tool. It is used to understand the world in a formative way [15]. Technology may change. Users may change. Tasks may change. The information system should overcome the fluctuation.
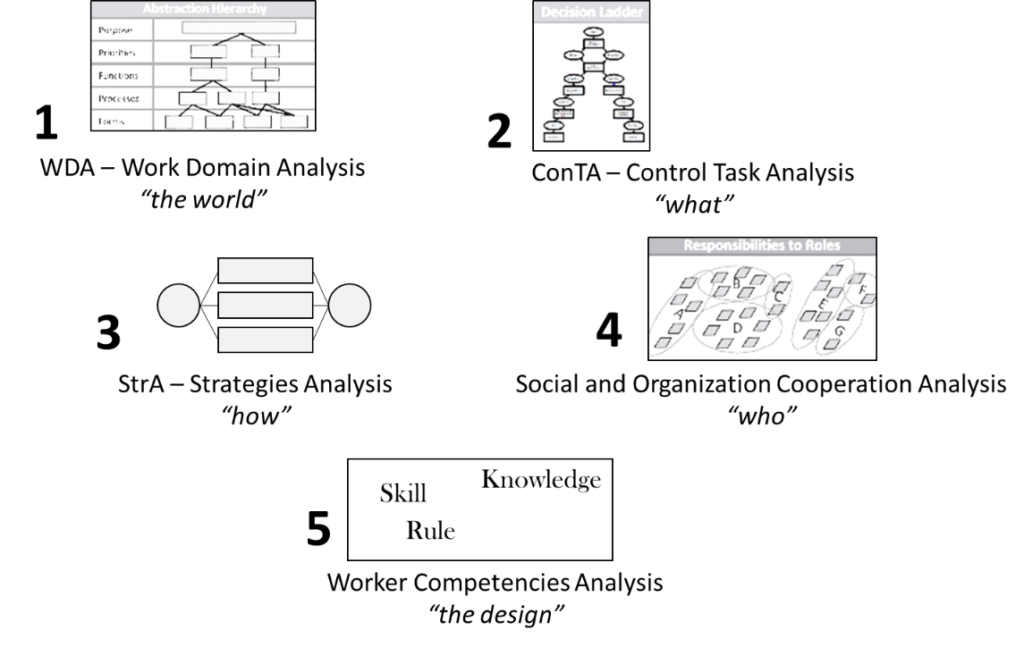
This modelling could be applied to the neuro-ICU. It requires 5 steps as shown in Figure 7.
The CWA framework includes five different phases : the work domain analysis (WDA) through the Abstraction Hierarchy (AH), the Control task (or activity) analysis which leads us to the decision ladder, the strategies analysis, the social organization and co-operation analysis, and the worker competencies analysis.
CWA will enable us to understand how the ICUs environment works and the different flows and parameters to take into account for the interface design. We will focus on the first point. The AH is the key tool in performing WDA and thus EID [14].
Work Domain Analysis (WDA) & Abstraction Hierarchy (AH)
As a first level of the CWA, WDA requires a description of domain through the AH as a first step of the designing project. In other words, we are defining the system of interest. This description is context independent. The analyses, and resultant diagrams, are not specific to any technology ; rather they represent the entire domain[15], [16].
The AH is a “treelike structure with multiple levels and each level are different from others and are ordered along a dimension”[14]. Each level has a means-ends link that can be answered by “how” and “why”.
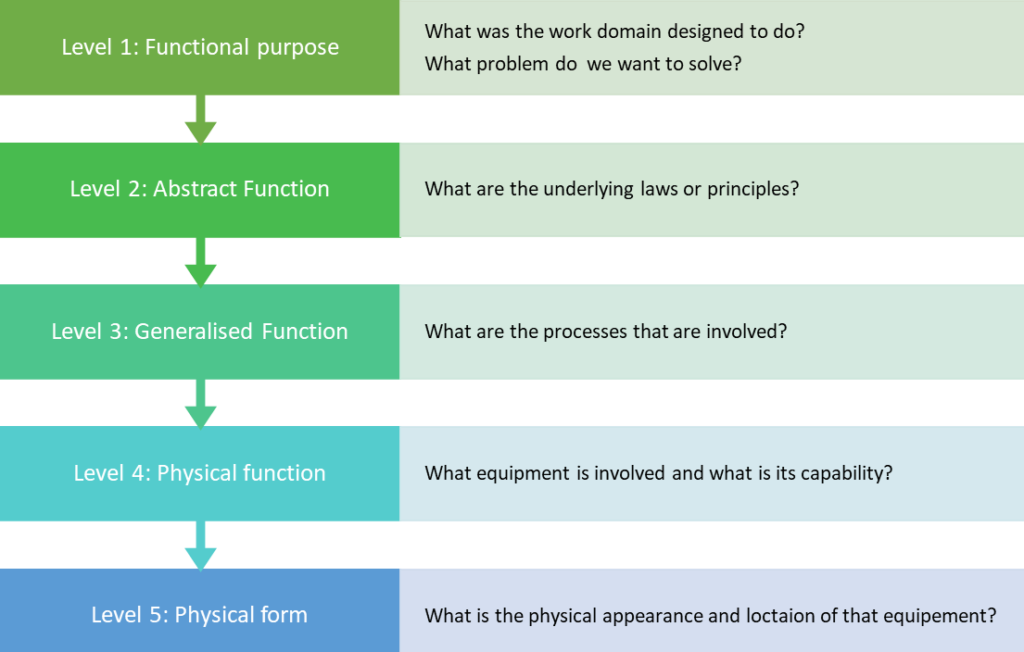
There are 5 steps, represented in Figure 8 : the functional purpose, the abstract function, the generalized function, the physical function and the physical forms. For each step, a question is to be answered.
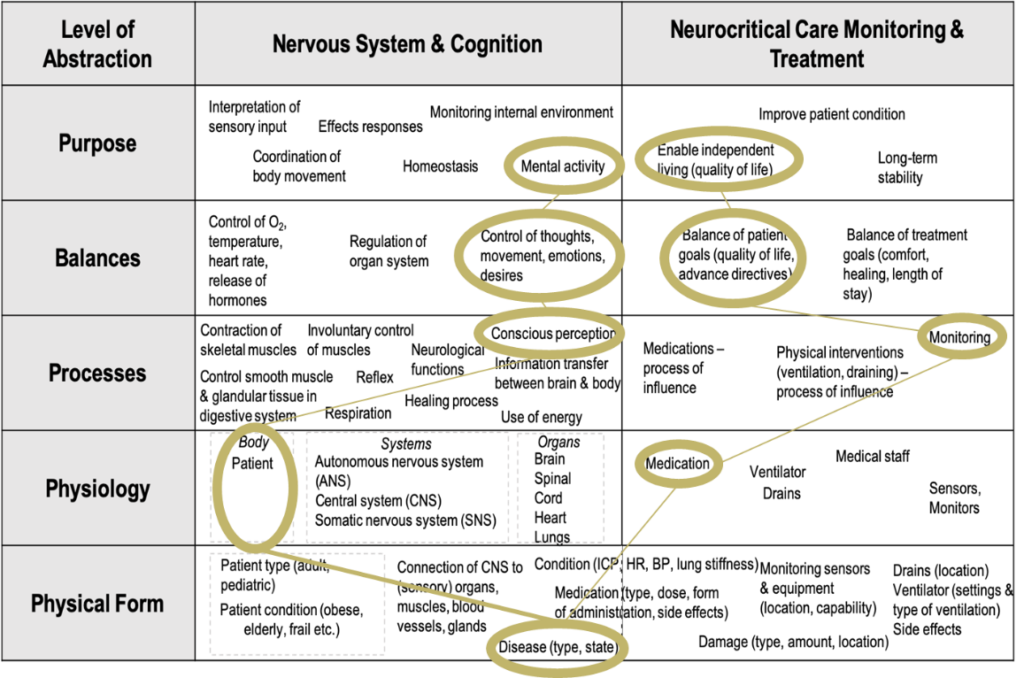
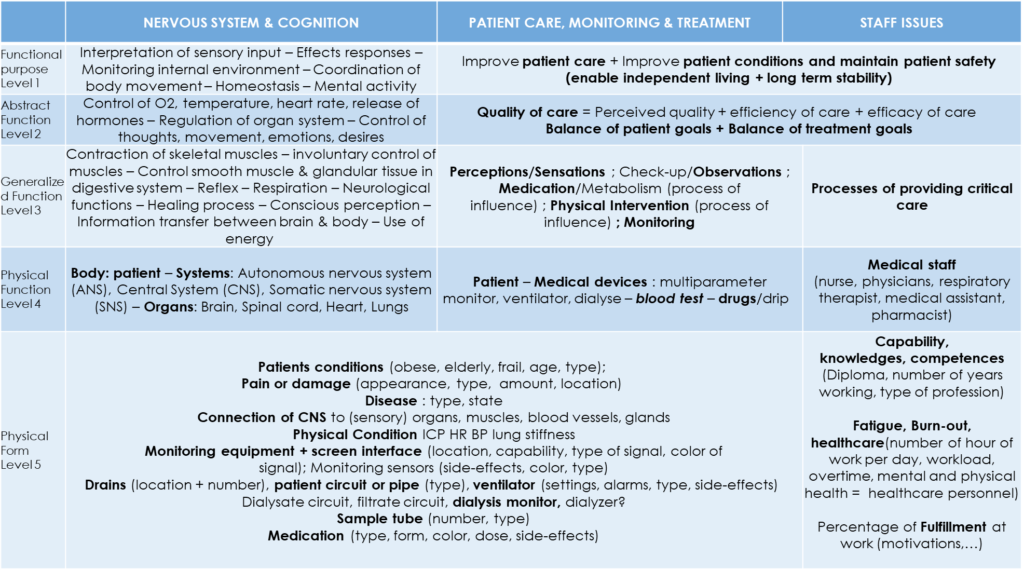
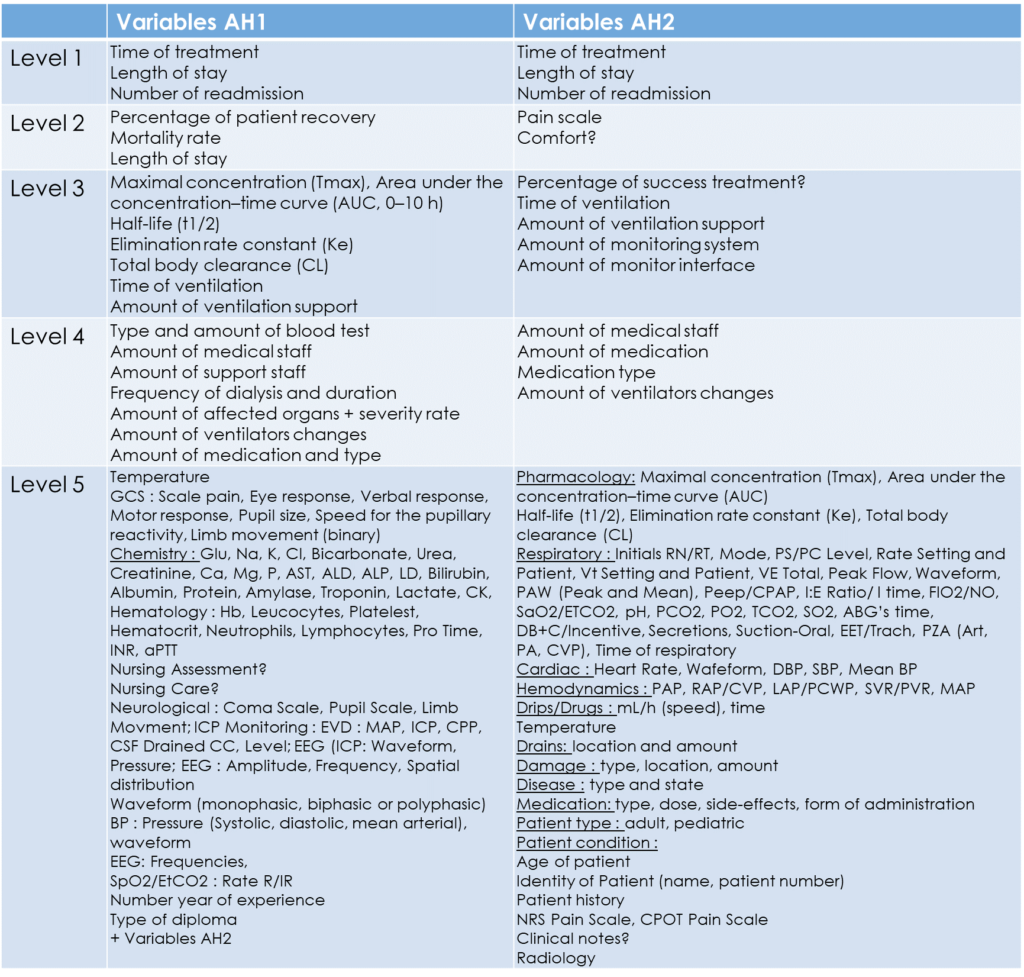
My collaborator, Ece, as a first step of the EID and through her observation at Hospital X, carried out previous work on the AH, in Figure 9. It focuses on the neuro-system and cognition as shown in Figure 9.
I contributed to this latter AH by focusing more on the quality of care and staff issues. As shown in Figure 10, an answer to the first question, what problem do we want to solve in ICU, would be to improve patient care, patient conditions and maintain patient safety. For each level, the AH is providing an answer to the question of each level of the AH.
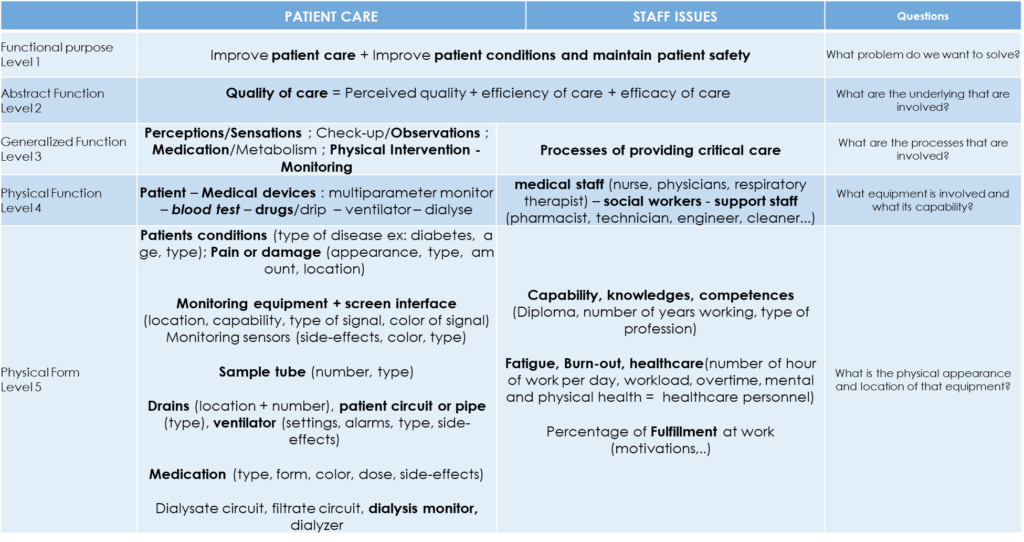
The quality of care is defined as the perceived quality, the efficiency and the efficacy of care. The perceived quality is, here, the level of quality of the care service as perceived by the patient in a more or less subjective way. By efficacy, we mean the ability to reach a goal of treatment by the physician, for example, whereas efficiency refers to the ability to reach this goal of treatment with the minimum waste of resources.
By their capability, knowledge or competences, the quality of care can be affected by the caregivers, and also by the fatigue, burn out or fulfillment at work.
Later, we merged both our AH into one describing widely the environment in Figure 11.
List of parameters
With the help of the AHs (Figure 10 and Figure 9), my collaborator, the brainstorming tool and the flowsheets for each level, we have listed all of the parameters and variables that could arise in Figure 12.
This list of parameters has been detailed in Appendix 1. For each parameter, we provided a definition, its units and range.
Focus on neuro-parameters
Three neurologic variables are important in neurocritical care and used in neuro-ICU : GCS, ICP and EEG.
Glasgow Coma Scale (GCS)
This is a neurological scale that aims to provide a reliable and objective way of recording the level of consciousness of a patient. The score lies between 3 to 15. Three elements are considered : Eye response (5 grades), Verbal response (5 grades) and Motor response (6 grades).
Intra-Cranial Pressure (ICP)
This is an invasive parameter. It represents the pressure applied by fluids such as CSF inside the skull and on the brain tissue. The CPP is the difference between the MAP and the ICP. Normal ICP lies between 5 to 10 mmHg [17]. IH, IICP or raised ICP is the most common clinical condition that requires treatment to reduce ICP.
Electroencephalogram (EEG)
This is a non-invasive parameter. It is the recording or measurement of cerebral bioelectric activity using electrodes placed on the scalp. It aims to monitor sedation or diagnosis of seizure activity. There exist 3 types of examinations : standard (short term), Holter (long term) and encephalic death. EEG is characterized by : Amplitude, Frequency, Spatial distribution and Waveform (monophasic, biphasic or polyphasic). There are 4 categories of frequencies : delta (<3.5Hz), theta (4 to 7.5 Hz), alpha (8 to 13 Hz) and beta (>13 Hz).
For each of these parameters, we tried to find out which companies sell these types of monitors and the available design screen types.
A first draft of the EID on Figma
After the results were obtained in this list of parameters and also from the observations my collaborator made during her time in the hospital, a first draft of the design was established on Figma, as shown in Figure 13.

Figma is a free collaborative interface design tool. Thanks to the UW, a free education version was available enabling us to work in team.
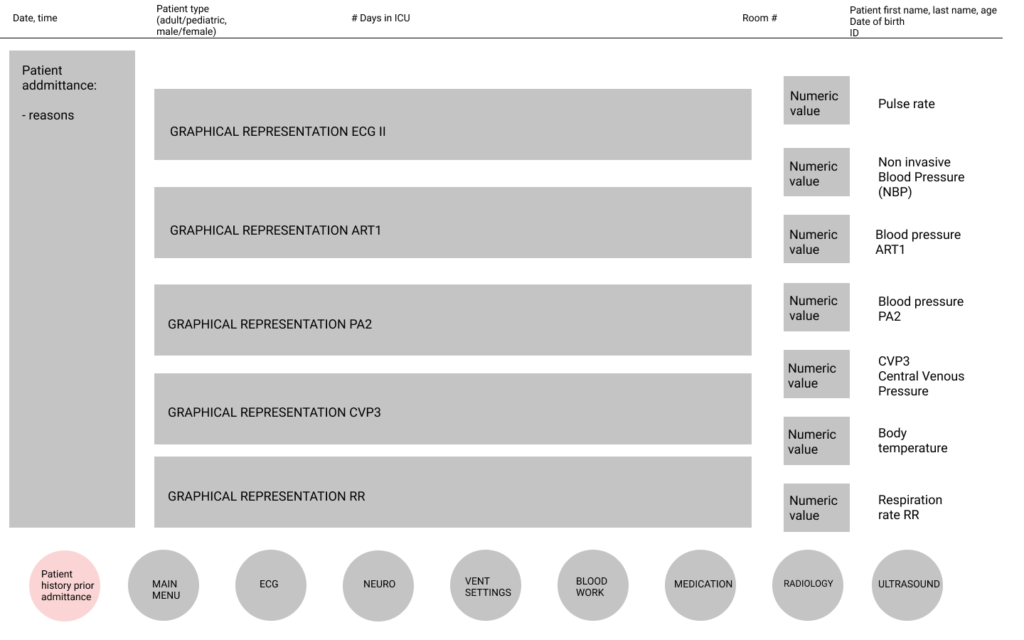
In order to take into account all persons likely to use this interface, a grayscale will be used. This is done specifically because there may be people with colour blindness within the nursing staff.
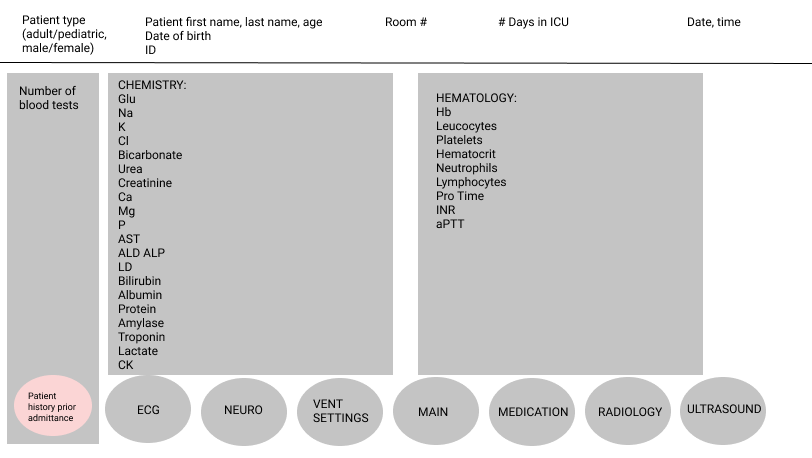
In Figure 14, the blood work parameters are presented as an example. In all screens, some important parameters are shown such as time, date, identification of the patient.
Feedback from the users : Personas and Scenarios
The next step was to understand the use cases. For that, we needed to understand clinicians better. Since we could not interview nurses and physicians due to the circumstances, we had to find another way to create scenarios and personas. We created personas to understand clinicians' perspectives and tasks/challenges. We researched on typical ICU scenarios to prepare for comparison and talked to a physician working at hospital X about them.
Personas
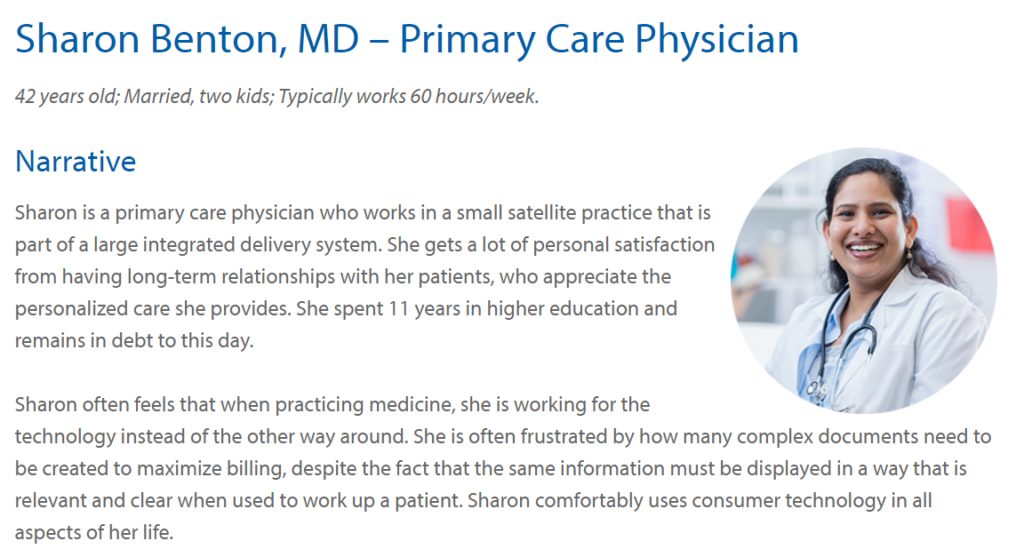
The goal here is to create reliable and realistic representations of our key audience segments for reference. The personas would be the clinicians that we are considering in our AH. We had to understand their perspectives and many examples were found online. Thanks to an opensource website, we got some personas which are listed in the Annexe II : Primary Care Physician, Hospital Nurse, Medical Assistant, Hospital Pharmacist, and an example in Figure 15.
A complete scenario would look like the whole process of a patient coming into the ICU with x problem. This would be something we give to our participants, so they can set all necessary parameters on the interface to treat the patient.
We created a list of scenarios. For each system, we have different cases with outcome variables, process variables and variables. The different mentioned systems are neurologic, pulmonary, cardiovascular, renal-fluid-electrolytes, gastro-intestinal-metabolic-nutrition and hematologic/infectious disease.
After a discussion with the physician, we obtained a list of the most critical case scenarios encountered in neuro-ICU. These are subarachnoid hemorrhage, intracerebral hemorrhage, acute ischemic stroke, traumatic brain injury, spinal cord injury and status epilepticus. We also obtained more relevant scenarios cases through simulation training databases. These scenarios cases would help to improve our EID.
3. Usability study
To have a better understanding of the boundaries of the existent software, a usability study will be done at hospital X in the fall or winter term.
Hospital X is currently using the software A of Company A as a bedside monitor. We found another new software B commercialized by Company B. This software only collects, visualizes, and stores ICU data in near real-time. It does not make any diagnosis. Software B can track data from software A through servers and uses the HL7[2] standard to communicate.
With my collaborator, we compared both technical parameters and functional parameters as well as the design differences in both displays. My collaborator has attended a demo of the new software B. Some of the limits of these two software are data storage, data tracking, visualization and alarms.
For example, we found out that real display size is typically between about 15” and 19”. At this moment, we adjusted the size of our EID draft.
The aim of this usability study is to compare the current ICU software A to the new software B. The findings of this study and the limits will help us in our EID in neurocritical care.
III. Personal feedback and career professional assessment of this internship
1. Personal feedback
This was my first experience in a non-European country. It was very exciting and interesting to discover the North American culture and especially Canadian one. It allowed me to improve my communication skills in English. This internship also gave me the opportunity to attend an international symposium on Human Factors and Ergonomics in Health care from May 18th to 21th 2020, which was done virtually due to the pandemic circumstances. It is worthy of mentioning that I also participated in the Fluxible online event, which was a Canadian UX Festival, on June 4th.
Moreover, I discovered the field of research, which I was apprehensive of previously. In particular, I was introduced to the field of design, in which I had no experience and knowledge prior to this internship.
Autonomy, freedom of planning, the pleasure of investigating in the health care field were the keys words that I retained from this experience. Teamwork allowed me to work in complementarity with my colleagues, each with different and complementary backgrounds.
In addition, we had to adapt ourselves to the changing sanitary requirements and Work from Home (WFH). Even though we could not interview the health personnel because they were needed most in the ICU, my research work was not affected. International solidarity linked to the pandemic made it easier for us to occasionally get free valuable online information about companies and medical devices. Working from home required us to have a balance between our personal and private life but also to have an efficient schedule allowing consistency.
Many thanks are due to our supervisor, Mrs. Burns, who organized weekly meetings and fostered effective communication with the members of the laboratory with the tools available. Furthermore, the UTC set up a support unit for isolated students during lock-down.
Despite the
quarantine, the first two months allowed me to meet and keep in touch with many
students from UW. It also made me aware of how lucky I was to live in France
and to have access to the university for free. We do not burden of study loan which
something I am grateful for. I am also grateful for the Eramus+ program otherwise
I wouldn’t have been able to embark on this journey.
2. Career objectives
Since my bachelor’s degree, I have had three different experiences in different settings : hospital, company/association and laboratory, which gives me a more complete vision of the types of trades in health engineering. This research internship opened me to the idea of finding a job in this field. Two aspects of biomedical engineering I missed were the contact with other people, especially the medical staff, and contact with medical devices. The job of an application engineer combines both. Also, it requires a lot of travel and I love to travel. Monitoring and cardiovascular are the areas in which I am particularly interested.
Conclusion
In neurocritical care, patients in ICU are in critical and sensitive states. As we have seen in Europe and also in America, the overload of ICUs during the pandemic was unexpected. In these cases, it is important for caregivers to make the best decisions during treatment as quickly as possible.
Through CWA modelling, our AH was able to lead us to the first draft of our EID. The second step of this project will be to apply the scenarios on this EID considering the second step of the CWA modelling : The Control Task Analysis, which is complementary to EID. This aims to take into account the decision ladder of the medical staff to help the physician with the diagnosis. A small mistake can jeopardize patient safety. The sooner we can diagnose the pathology, the better the treatment plan would be meaning enabling a better quality of care.
Bibliographic references
[1] Heath Kelly, ‘The classical definition of a pandemic is not elusive’, WHO, doi : 10.2471/BLT.11.088815.
[2] Jamie Ducharme, ‘World Health Organization Declares COVID-19 a “Pandemic.” Here’s What That Means’, Time, Mar. 11, 2020.
[3] Oxford Dictionary, ‘Definition of Epidemic’, https://www.lexico.com/. Accessed : Jun. 28, 2020. [Online]. Available : https://www.lexico.com/en/definition/epidemic.
[4] World Health Organization, ‘Technical guidance : Naming the coronavirus disease (COVID-19) and the virus that causes it’. Accessed : Jun. 28, 2020. [Online]. Available : https://www.who.int/emergencies/diseases/novel-coronavirus-2019/technical-guidance/naming-the-coronavirus-disease-(covid-2019)-and-the-virus-that-causes-it.
[5] World Health Organization, ‘Coronavirus disease (COVID-19) pandemic’, https://www.who.int/. https://www.who.int/emergencies/diseases/novel-coronavirus-2019 (accessed Jun. 28, 2020).
[6] World Health Organization, ‘Q&A on coronaviruses (COVID-19)’, https://www.who.int/, Apr. 17, 2020. https://www.who.int/news-room/q-a-detail/q-a-coronaviruses (accessed Jun. 28, 2020).
[7] Celiac Disease Foundation, ‘Celiac Disease and COVID-19’, Celiac Disease Foundation. https://celiac.org/celiac-disease-and-covid-19/ (accessed Jun. 28, 2020).
[8] Research Infosource Inc., ‘Canada’s Top 50 Research Universities 2019’, 2019. https://researchinfosource.com/top-50-research-universities/2019/top-research-universities-by-tier-corp (accessed Jun. 28, 2020).
[9] ‘UW, University of Waterloo’, University of Waterloo, Nov. 03, 2016. https://uwaterloo.ca/content/home (accessed Jun. 28, 2020).
[10] Macleans.ca, ‘Canada’s best universities by reputation : Rankings 2020’, https://www.macleans.ca/, Oct. 03, 2019. https://www.macleans.ca/education/canadas-top-school-by-reputation-2020/ (accessed Jun. 28, 2020).
[11] ‘QS Graduate Employability Rankings 2019’, Top Universities, Feb. 01, 2017. https://www.topuniversities.com/university-rankings/employability-rankings/2019 (accessed Jun. 28, 2020).
[12] ‘Centre for Bioengineering and Biotechnology, CBB Team’, Centre for Bioengineering and Biotechnology, Jun. 18, 2015. https://uwaterloo.ca/bioengineering-biotechnology/about/people/cbb-team (accessed Jun. 28, 2020).
[13] CIHI, Canadian Institute for Health Information, ‘Care in Canadian ICUs’, Aug. 2016. Accessed : Jun. 28, 2020. [Online]. Available : https://secure.cihi.ca/free_products/ICU_Report_EN.pdf.
[14] Catherine M. Burns and John R. Hajdukiewicz, Ecological Interface Design. CRC Press, 2004.
[15] K. J. Vicente, Cognitive Work Analysis : Toward Safe, Productive, and Healthy Computer-Based Work. CRC Press, 1999.
[16] J. Rasmussen, ‘The role of hierarchical knowledge representation in decisionmaking and system management’, IEEE Trans. Syst. Man Cybern., vol. SMC-15, no. 2, pp. 234–243, Mar. 1985, doi : 10.1109/TSMC.1985.6313353.
[17] C. A. Mount and J. M Das, ‘Cerebral Perfusion Pressure’, in StatPearls, Treasure Island (FL): StatPearls Publishing, 2020.
[18] ASTM International, ‘Annex B of ASTM Standard F2761-09 : Clinical Context and Clinical Scenarios’. 2013, Accessed : Jun. 28, 2020. [Online]. Available : http://www.mdpnp.org/uploads/Clinical_Scenario_and_CConOps_definitions_and_framework.pdf.
Annexes
Annex I - List of parameters
| List of Parameters | Definition | Units | Range |
| Time of treatment | The time between the first and the last treatment order. | Seconds, Minutes, Hours, Days, Months, Years | Not determinable (depends on the patient) [0:∞[ |
| Length of stay | The time between patient arrival and discharge of the ICU. | (Seconds), Minutes, Hours, Days, Months, Years | Not determinable (depends on the patient) [0:∞[ |
| Readmissions | The number of times being admitted to an ICU again. | 0, 1, 2, 3, … (positive integer) | Not determinable (depends on the patient) [0:∞[ |
| Patient recovery | Which criteria include the patient recovery ? | % | [0:100] |
| Mortality rate | The relation between alive and dead patients in the number of deaths in ICU. | % | [0:100] |
| Comfort in the ICU | To be defined with criteria : Type/size of roomType of bedHospital mealSingle or shared room | % | [0:100] |
| Severity rate | The amount of affected organs by disease. | % | [0:100] |
| Pain scale | |||
| NRS : Numeric Rating Scale | 0 : No pain 10 : Worst pain possible | [0:10] | |
| CPOT : Critical Care Pain Observation Tool | 3 : No pain 12 : Maximum Pain | [3:12] | |
| GCS : Glasgow Coma Scale | Neuro | 3 : No pain 15 : Maximum Pain | [3:15] |
| Respiratory parameters | |||
| Time of ventilation | The time between starting and stopping the mechanical ventilation on the patient. | Seconds, Minutes, Hours | [0:∞[ |
| Ventilation support | The amount of how much the patient is supported by mechanical ventilation. | % 0 : the patient breathes by him-/herself 100 : ventilator supplements respiratory function | [0:100] |
| Ventilator changes | The amount of how many times the patient circuit is changed to a different setting. | 0, 1, 2, 3, … (positive integer) | Not determinable (depends on the patient) [0:∞[ |
| Respiratory rate (f) | The number of breaths per minute or, more formally, the number of movements indicative of inspiration and expiration per unit time. | b/m | 10-20 |
| Tidal volume (Vt) | The volume of air moved into and out of the lungs during each ventilation cycle. | Ml/kg | 5-15 |
| Oxygen concentration (FiO2) | The percentage or concentration of oxygen that a person inhales. | % | b/w 21-90 |
| I:E ratio | The ratio of inspiratory time : expiratory time. | X | 1:2 |
| Flow rate or peak inspiratory flow rate | The maximum flow at which a set tidal volume breath is delivered by the ventilator. | L/min | 40-100 |
| Sensitivity/trigger | Determines how much effort the patient has to exert before his inspiration is augmented by the ventilator. | cmH2O | 0.5-1.5 |
| Pressure Limit | cmH2O | 10-25 | |
| PEEP | Abbreviation for positive end-expiratory pressure. A method of ventilation in which airway pressure is maintained above atmospheric pressure at the end of exhalation by means of a mechanical impedance, usually a valve, within the circuit. | cmH2O | 5-10 |
| Other parameters | VC NIF Cuff pressure Extubated VENT ETT/Trach size Taped Air Entry Adventitious Sounds Initials RN/RT, Mode, PS/PC Level, Rate Setting and Patient, Vt Setting and Patient, VE Total, Peak Flow, Waveform, PAW (Peak and Mean), CPAP, I time, FIO2/NO, SaO2/ETCO2, pH, PCO2, PO2, TCO2, SO2, ABG’s time, DB+C/Incentive, Secretions, Suction-Oral, EET/Trach, PZA (Art, PA, CVP), Time of respiratory (These depend on the ventilator). | Cm Numeric Scale(Air Entry) Scale Scale | 0, 1, 2, 3 +, ++, +++ 1 2 3 M P B |
| Monitoring parameters | |||
| Monitoring systems | Number of different type of monitors. | 0, 1, 2, 3, … (positive integer) | ND |
| Monitor interfaces | Number of different monitor screens. | 0, 1, 2, 3, … (positive integer) | ND |
| Body temperature | The temperature measured on a patient’s body. | °K or °C | 98.6°F or 37°C |
| Cardiac/ECG | Heart Rate, Waveform, Diastolic BP, Systolic BP, Mean BP | Beats per minute (bpm) mmHg mmHg | from 60 to 100 lower than 80 (60) 120-129 (110) (76,67) |
| Hemodynamics | PAP Pulmonary Artery Pressure RAP Right Atrial Pressure /CVP LAP Left Atrial Pressure /PCWP SVR Systemic Vascular Resistance /PVR MAP Mean Arterial Pressure | mmHg mmHg mmHg dynes · sec/cm5 mmHg | 15 – 25 2-6 6-12 800 – 1200 70 – 105 |
| ICP Monitoring (EVD) | MAP Mean Arterial Pressure ICP Intra Cranial Pressure CPP Cranial Perfusion Pressure CSF Drained CC : Cerebro Spinal Drained Level | mmHg mmHg mmHg Cubic Centimer Cubic Centimer | MAP = CPP – ICP = 70 – 10 = 60 5 to 15 (10) 60-80 (70) |
| EEG | Amplitude, Frequency, Spatial distribution Waveform | µV Hz | about 100 on the scalp delta (<3.5Hz) theta (4 to 7.5 Hz) alpha (8 to 13 Hz) beta (>13 Hz) monophasic, biphasic or polyphasic |
| SpO2 | Rate R/IR Percentage of oxygen Saturation | % | >95 |
| EtCO2 | mmHg | 35-45 | |
| Blood test parameters | |||
| Blood tests | Number of sample tubes required for the tests. | 0, 1, 2, 3, … (positive integer) | |
| Type of blood test | Chemistry : Glu, Na, K, Cl, Bicarbonate, Urea, Creatinine, Ca, Mg, P, AST, ALD, ALP, LD, Bilirubin, Albumin, Protein, Amylase, Troponin, Lactate, CK, Creatinine Kinase Hematology : Hb, Leucocytes, Platelest, Hematocrit, Neutrophils, Lymphocytes, Pro Time, INR, aPTT | concentration mg/dL mEq/L mmol/L mEq/L mmol/L mg/dL mg/dL mg/dL mmol/L or mg/dL mg/dl U/L ng/dL U/L U/L mg/dL g/dL g/dL U/L ng/mL mmol/L SI units/L mmol/L mmol/L /L mg/Dl mmol/L /L | https://webpath.med.utah.edu/EXAM/labref.htm [70:100] [135 :145] [3.6:5.2] [98:106] [23:29] [6:20] [0.9:1.3] ♂ [0.6:1.1] ♀ fr 18:60 yo [8.6:10.2] 0.6-1.1 or 1.46–2.68 3.4 to 4.5 14 - 59 2 - 9 50-100 300 - 600 less than 0.3 3.5 - 5.2 6.3 - 8.2 40-140 <0.4 0.5-1 ♂ 55-170 ♀30-135 ♂8.7-11.2 ♀7.4-9.9 135 – 145 150-400 x 10^9 6 and 20 135 – 145 1.0-4.0 X 109 https://mcc.ca/objectives/normal-values/ |
| Pharmacology parameters | |||
| Medication amount and types | Number of different types of medication and names | 0, 1, 2, 3, … (positive integer) and name | [0:∞[ |
| Maximal concentration (Cmax or Tmax) | Cₘₐₓ is the maximum serum concentration that a drug achieves in a specified compartment or test area of the body after the drug has been administered and before the administration of a second dose. | Unit of concentration | Drug-depended |
| Area under the concentration–time curve (AUC, 0–10 h) | The area under the curve (AUC) is the definite integral of a curve that describes the variation of a drug concentration in blood plasma as a function of time. | Unit of concentration | Drug-depended |
| Half-life (t1/2) | The time it takes for the concentration of the drug in the plasma or the total amount in the body to be reduced by 50%. | Units of time | Drug-depended |
| Elimination rate constant (Ke) | It is a value that describes the rate at which a drug is removed from the system. | Units of concentration | Drug-depended |
| Total body clearance (CL) | The total body clearance (ClT) is the sum of the renal clearance (see the record on Renal drug excretion), hepatic clearance, and clearance due to any other routes of elimination (respiratory, fecal, salivary, etc.). Clearance is a measure of the efficiency of the body to eliminate the drug. | Unit of concentration | Drug-depended |
| Dose of medication | Amount of medication taken at one time. | ml | Drug-depended |
| Dosage of medication | Frequency of doses over specific period of time. | 0, 1, 2, 3, … (positive integer) | [0:∞[ |
| Side-effects of medication | Enter the observed and diagnosed side-effects of given medication. | Drug-depended | |
| Drips/Drugs | mL/h | Drug-depend | |
| Location and amount of drain | Location of drain on patient’s body and the amount of drains used. | Areal description of body 0, 1, 2, 3, … (positive integer) | Depends on the patient’s conditions |
| Dialysis parameters | |||
| Frequency of dialysis | Each time that we change the dialysis circuit. | 0, 1, 2, 3, … (positive integer) | Not determinable (depends on the patient) [0:∞[ |
| Total duration of dialysis | Temporal description of the duration of dialysis application on patient. | Seconds, Minutes, Hours, Days | (Depends on the patient) [0:∞[ |
| URR | Urea reduction ratio | % | >65 |
| Kt/V | Another way of measuring dialysis adequacy K stands for the dialyzer clearance, the rate at which blood passes through the dialyzer, expressed in milliliters per minute (mL/min)t stands for timeKt, the top part of the fraction, is clearance multiplied by time, representing the volume of fluid completely cleared of urea during a single treatmentV, the bottom part of the fraction, is the volume of water a patient's body contains | Below 1.2 | |
| Other Neurologic parameters | |||
| Pupil size | Diameter measured of pupils with variance of light brightness. | mm | from 2 to 4 mm in diameter in bright light to 4 to 8 mm in the dark |
| Reactivity of pupil | Pupil’s accommodation to light changes. | Binary | Yes or No |
| Limb movement | Ability to move limbs. | Left or Right, Scale for Legs and Arms | Yes or No, 0, 1, 2, 3, 4, 5 Posturing F/E |
| Patient stats | |||
| Damage (type, location, amount) | Observed and diagnosed patient’s body damage type, location and the amount of damages. | Text | |
| Disease (type and state) | Diagnosed disease type and state of disease. | Text | |
| Patient type | Description of patient (pediatric, adult). | adult, pediatric | |
| Patient conditions | Description of diagnosed conditions. | Text | |
| Patient identity | Name, age, patient ID. | Text, number, number | Text, [0:120[, [0:∞[ |
| Patient history | Available information on patient’s history from GP, other hospitals and treatments. | Text | |
| Imaging setting | |||
| Radiology (DICOM?) | Images taken (Scans etc.) | Image file | |
| Notes and Assessment | |||
| Clinical notes | Notes taken by physicians to keep track of the requirements for further treatment. | Text | |
| Nursing Assessment | Patient assessment taken by nurses. | Text | |
| Staff parameters | |||
| Medical staff (in ICU) | Number of nurses, therapists, physicians, radiologists, ... | 0, 1, 2, 3, … (positive integer) | ND |
| Support staff (in ICU) | Number of pharmacists, technicians, engineers etc. | 0, 1, 2, 3, … (positive integer) | ND |
| Years of experience | Time that shows how long a staff member has worked in a specific/related field. | 0, 1, 2, 3, … (positive integer) | |
| Type of diploma | Graduated degree of staff. | Nurse, pharmacist, physicians | |
| Important parameters | |||
| Date | Day of the year. | Year/Month/Day | |
| Time | Clock time. | Hours, Minutes, Seconds |
References :
Ventilator Parameters : https://www.slideshare.net/sanilmlore/mechanical-ventilation-29439357
Hemodynamics : http://www.lidco.com/education/normal-hemodynamic-parameters/
Annex II - List of personas
| PERSONAS | Primary Care Physician https://www.ehra.org/resource-library/personas/sharon-benton-md-primary-care-physician | Hospital Nurse https://www.ehra.org/resource-library/personas/carolyn-coolridge-rn-hospital-nurse | Medical Assistant https://www.ehra.org/resource-library/personas/mary-michaels-medical-assistant | Hospital Pharmacist https://www.ehealthireland.ie/Strategic-Programmes/Electronic-Health-Record-EHR-/Final-Persona-Scenario-files/Acute-HSP-Hospital-Pharmacist-Charlene-Hunter-v1-0.pdf |
| Name | Sharon Benton, MD | Carolyn Coolridge, RN | Mary Michaels | Charlene Hunter |
| Short presentation about them | 42 years old ; Married, two kids ; Typically works 60 hours/week | 45 years old ; married, three children ; BSN degree ; Works four 10-hour shifts per week, plus occasional weekend overtime. | Age 35 ; Married, two children ; Associate's degree, healthcare administration ; Works full-time, Monday – Friday | 40 years married with 2 young children MSc in Pharmacy |
| Tasks | Log into HERTake in charge new drug prescriptionNeed to check medication history Inpatient prescription chartReview the record of the patient Communicate with the medical team through HER for recommendationComplete pharmacological review | |||
| Short-term goals | share information about my patients with other providers efficiently and easilyspend less time completing administrative or duplicative taskscommunicate effectively with patients pay educational debt and support family.a better work-life balance | Ensure that all patients receive their medications and other treatments on timeEducate patients on a healthy lifestyle and observe the patient putting the education into actionMake sure each patient and family feels like they are getting the care and attention they need.Organize the day to finish shift on time.Complete all tasks. Ensure patients are discharged in a timely manner see and communicate easily each patient’s plan of care | Make a patient feel better todayGet all the patients out on time todayDocument the most accurate patient information Help patients access the right information about their treatment plansGet additional EHR[3] training to increase workflow efficiency. | Counsel the patients on the safe use of prescribed products Participate in departmental audits |
| Long-term goals | provide high-quality care for patients consistently, see improvements in their outcomes, and help them stay healthy. Identify new revenue opportunities at the practice and participate in an advanced care team solution Identify more ways that technology can be used in the practice to save time or improve processes, workflows and tasks.Become a totally paperless medical practice in the next two years. | Become proficient in customization and optimization of EHR to improve daily workflow.Seamlessly capture data during routine provision of care Stay up-to-date on continuing education required to maintain RN licensure every two years.Develop and implement a training program for new graduates and other nurses new to our unit to help them get up to speed more quickly and efficiently. | Go back to school to become a nurseCreate an environment that makes our office run more smoothly and makes patients feel more comfortable. | |
| Typical problems | Spend 2–4 hours every day after work completing EHR tasksThe practice cannot keep exam rooms full, because of completing the post-visit quality reporting tasks required for each patient.Daily frustrations when interacting with the EHR system because of many clicks required for frequently used workflows, navigation is difficult, and the system does not organize the data in an efficient way Prior authorization and other payer-imposed roadblocks contribute to inefficient care delivery for both clinicians and patients.Patients with multiple chronic conditions can be very difficult to care for. | Staffing shortages can put nurses at greater risk for patient safety issues.Unable to locate patient records in one place.High percentage of nursing burnout, with nurses leaving the patient care workforce in favor of non-direct patient care types of nursing.Unable to speak to some patients without interpreter due to language barrier.Difficulty communicating with healthcare team efficiently Spend a lot of time recording large amounts of information and completing documentation.Common tasks can be laborious (too much clicking).The doctor keeps reconciling the meds incorrectly, further lengthening the time required to discharge patients.Rarely doing one task at a time and constantly interrupted. pressure and fatigueno consistency. Misuse from other nurses of HER (completing the same info in a different part)Complex tasksMedication management Can’t easily see what is missing or what hasn’t been done, particularly around documentation.Lack of investment in daily patient because of dissatisfaction of jobInjuries | Don’t feel efficient with this EHRMust cater to each doctor’s work habits and documentation styles.Possibilities for errors.Interruptions and distractions.Inexperienced staff/high turnover.Wear too many hats.Spend a lot of time with tasks that should be faster/easier. | Frustration because of the lack of computers on the wardsNot having enough time to provide safe and effective cover on the wards as well as undertake her dispensary duties |
[1] The SHAP is a method used to explain individual predictions based on the game theoretically optimal shapley values. It was introduced by Lundberg and Lee in 2016.
[2] HL7 is an international standard that is used to transfer data between software applications. It is used by different healthcare providers.
[3] E.H.R.: Electronic Health Record
